There are 2 main types of GBS infection in newborns. Rupture of membranes IV.
 Treating Babies For Gbs Infection Group B Strep Support
Treating Babies For Gbs Infection Group B Strep Support
ACOGs guidance replaces the 2010 guidelines published by CDC.

Gbs positive newborn. In June 2019 the American College of Obstetricians and Gynecologists ACOG published a new Committee Opinion Prevention of Group B Streptococcal Early-Onset Disease in Newborns external icon which all obstetric care providers should now be following. In this study we aimed to determine the GBS colonization rate amo. Intrapartum antibiotic prophylaxis intravenous ROM.
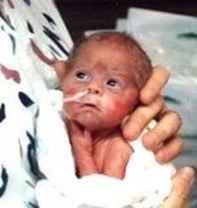
In this article we will focus on early infection which occurs in the first 7 days after birth. Signs of sepsis in newborn at birth. GBS disease is most common in newborns.
Group B Streptococcus IAP. The Group B Streptococcus GBS 2 Streptococcus agalactiae Group B Streptococcus GBS is a Gram-positive beta-hemolytic microorganism that colonizes the human lower Gastro Intestinal and Genital tracts GBS can cause life-threatening infections in neonates and in immuno-compromised adults Mother to Infant Transmission. Testing positive for GBS bacteria late in pregnancy.
When a baby has an early GBS infection symptoms usually appear within the first 12 hours and almost all babies will have symptoms within 24-48 hours CDC 2010. Positive maternal GBS culture AT ANY POINT during THIS pregnancy 2. If your test results come back positive your healthcare provider will likely give you intravenous antibiotics during labor.
The rate of positive GBS cases is declining in Australia due to preventative screening programs in most hospitals when the mother is around 37 weeks pregnant. Early infection and late infection. GBS status unknown within 5 weeks of delivery AND either--.
While having GBS wont classify your pregnancy as high risk GBS does increase a pregnant womans chances of developing. While composite adverse maternal outcomes occurred in 9 666 31 859 and 5 1087 in the GBS-positive GBS-negative and. Or Streptococcus agalactiae is gram-positive diplococcus that is a common colonizer of the gastrointestinal and genital tracts.
Newborn care FBC and observe for 48 hours All newborn babies CS. Greater than or equal to. In the case of dealing with GBS and newborns there is evidence that using antibiotics actually increases the chance the newborn will become ill source unknown see comments below and not just from GBS.
Risk Factors For GBS Infection. Early onset Group B Streptococcal disease FBC. E-coli and other antibiotic-resistant bacterial strains can.
GBS-Negative groups 067 95 CI 030150. There are additional times your health care provider may suggest you are tested for GBS especially if the baby may be at greater risk to exposure to GBS if the mother is infected. Indications for Intrapartum Prophylaxis see table 3 A B G 1.
The top three maternal factors associated with positive neonatal GBS infections were the presence of symptomssigns of maternal infection dysfunctional labor and fetal distress. Group B Streptococcus GBS. The bacteria can be transmitted to the newborn before and during birth and cause early-onset neonatal disease.
A positive test result for GBS by culture DNA probe or NAAT performed during antenatal screening indicates colonization and the woman should receive IAP. Greater than less than. However infants with early-onset GBS can be born to women with negative antenatal screening results because all laboratory-screening methods are imperfect.
Developing a fever during labor. In newborns the major manifestations of GBS infection are congenital pneumonia sepsis and meningitis. Adverse neonatal outcomes were observed in 8 59 31 86 and 2 43 in the GBS-positive GBS-negative and unknown groups respectively P 0530 Odds Ratio between GBS-Positive vs.
Among the 1532 maternal GBS carriers 18 gave birth to infants with early-onset GBS disease which occurred within 1 day after birth resulting in a vertical. GBS colonization in pregnant women is generally asymptomatic. Having 18 hours or more pass between when their water breaks and when their baby is born.
However maternal colonization is the primary risk factor for GBS infection in neonates and young infants 12. Being GBS positive doesnt mean that your newborn baby will be at risk of becoming sick from it. Rectovaginal area of pregnant women can be colonized transiently with group B Streptococcus GBS without causing disease.
This can reduce the chance of you passing the bacteria onto your child if you have a vaginal delivery. In pregnant women GBS infection may cause urinary tract infection sepsis chorioamnionitis postpartum endometritis pelvic thrombophlebitis and endocarditis. Full blood count GBS.
GBS bacteriuria during current pregnancy 3. Prior infant with GBS disease 4. There are factors that can increase a pregnant womans risk of having a baby who will develop GBS disease including.
A urinary tract infection UTI an infection of the bloodstream called sepsis an infection of the uterine lining.
 How To Help Protect Your Baby Group B Strep International
How To Help Protect Your Baby Group B Strep International
 How To Help Protect Your Baby Group B Strep International
How To Help Protect Your Baby Group B Strep International
 Group B Strep A Danger To Infants Gbs Awareness Month Sepsis Alliance
Group B Strep A Danger To Infants Gbs Awareness Month Sepsis Alliance
 My Full Term Group B Strep Birth Story Life With Pink Princesses Youtube
My Full Term Group B Strep Birth Story Life With Pink Princesses Youtube
What You Should Know About Gbs Mommytobeprep Com
 Poster Signs And Symptoms Of Group B Strep Infection In Babies
Poster Signs And Symptoms Of Group B Strep Infection In Babies
 Group B Strep Meningitis Meningitis Now
Group B Strep Meningitis Meningitis Now
 How To Help Protect Your Baby Group B Strep International
How To Help Protect Your Baby Group B Strep International
 The Facts About Group B Strep In Pregnancy Leaflet By Group B Strep Support Issuu
The Facts About Group B Strep In Pregnancy Leaflet By Group B Strep Support Issuu
 Group B Strep Gbs Resources Healthy Newborn Network
Group B Strep Gbs Resources Healthy Newborn Network
 Group B Strep What Does It Mean For Me And My Baby Holistic Health Healing Pregnancy Through Birth Postpartum Services For All Settings
Group B Strep What Does It Mean For Me And My Baby Holistic Health Healing Pregnancy Through Birth Postpartum Services For All Settings
The Jesse Cause Saving Babies From Group B Strep


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.